Acne Vulgaris is a serious issue

Introduction

Acne is also known as a pimple in layman’s terms.
Acne Vulgaris is one of the most common skin disorders – if not common, it has been evident in 70% of the population at some stage during their adolescence, occurs mainly due to occlusion of the sebaceous gland which may be due to hair, sebum, and dirt including bacteria and dead skin cells.
It’s a chronic inflammatory disease of the pilosebaceous unit.
Open pores when gets blocked usually present as open comedones (blackhead) and closed come dome (white head).
About 80% of people ages 11 to 30 will have some or the other mild form of acne, and most people are affected by it at some point in their lives.
Area affected mostly includes the face, arms, chest, and upper back.
Pathophysiology of acne
Acne occurs due to the involvement of the sebaceous gland, as well as the pro-inflammatory activity of the cutaneous microbiome.
- The pathophysiology involves three actors, hyper seborrhoea, abnormal follicular keratinization, and Propionibacterium acnes proliferation in the pilosebaceous unit.
- As a result of their interaction, the cutaneous microenvironment changes and leads to inflammatory reactions of the host that foster acne lesion progression.
- It involves different factors resulting in inflammation and the formation of different types of acne lesions.
- These factors include the quantitative and qualitative alteration of the sebum during puberty, called dysmenorrhoea, triggered by internal factors such as hormonal or genetic factors, and external factors such as comedogenic cosmetics, aggressive detergents or drugs, which may stimulate mechanisms involved in the pathophysiologies of acne.
- The impact of stress and diet on dysmenorrhoea remains to be elucidated. Sebum production is induced by different receptors expressed by the sebaceous gland. In addition to the well-described histamine receptor activated by histamines, the hormonal DHT receptor, activated by androgens, and the neuromodulator receptor, mainly substance P and corticotrophin-releasing hormone (CRH) receptor which are mainly activated by stress.
- Therefore, increased sebum excretion, alteration of lipid composition, and the oxidant/antioxidant ratio characteristic of the skin surface lipids are major concurrent events associated with the development of acne. If sebum interferes with the process of follicular keratinization in the pilosebaceous unit, pore blockage may occur, contributing to lesion formation and acne.
- Extreme caloric restriction dramatically decreases the sebum excretion rate and these changes can be reversed when a normal diet is resumed. Various studies have demonstrated that increased consumption of dietary fat or carbohydrate increases sebum production and modifications to the type of carbohydrate can also alter sebum composition. o Typical western diet, comprised of milk and hyperglycaemic foods, may have potentiating effects on serum insulin and insulin-like growth factor-I (IGF-I) levels, thereby promoting the development of acne.
- There is an association between the local overproduction of active androgens and acne.
- Acne patients produced higher rates of testosterone and 5α-dihydrotestosterone (5α-DHT) in their skin than healthy individuals. High testosterone levels have been implicated with enhanced sebaceous gland activity in humans and consequently with diseases marked by hyper seborrhea, such as Acne vulgaris. However, only a few patients with androgenic disorders exhibit hyperandrogenemia, an observation that indicates the predominance of peripheral tissue events for the occurrence of clinical signs.
- Dehydroepiandrosterone (DHEA) has been also shown to regulate sebum production, especially in postmenopausal women. Consequently, several researchers have suggested the use of DHEA as an anti-aging agent. However, in in vitro experiments DHEA has been shown to have no direct effect on the biological activity of human sebocytes
- Inflammation is regarded as a key component of the pathogenesis of acne.
- An increase in IL-1 activity occurs before the hyperproliferation around uninvolved follicles and this triggers the activation of the keratinocytes
Therefore, we can sum up the factors that can cause acne and/or make it worse:
- Fluctuating hormone levels around the time of a woman’s period.
- Picking at acne sores.
- Clothing and headgear, like hats and sports helmets.
- Air pollution and certain weather conditions, especially high humidity.
- Using oily or greasy personal care products (like heavy lotions, creams, or hair pomades and waxes) or working in an area where you routinely come in contact with grease (such as working at a restaurant where there are greasy food surfaces and frying oil).
- Stress, which increases the hormone cortisol, can also cause acne to flare.
- Certain medications.
- Genetics.
Clinical features
- It is largely a hormonal condition that’s driven by androgen hormones, which typically become active during the teenage and young adult years. Many people continue struggling with acne into their 20s, 30s, and beyond. Some even develop acne for the first time as adults.
- The most common spots of acne are over the face, forehead, chest, shoulders, and upper back. Oil glands are all over your body, but those are the places where there are the most. Female patients may more frequently develop lesions on the lower third of the face, especially on the chin and jawline.
- Acne lesions range from comedones to papules and pustules, cysts, and/or nodules. In one study of post-adolescent acne, 85% of patients had mostly come donal acne with two subtypes identified as persistent and late-onset acne. Persistent acne, which is defined as acne that persists beyond adolescence into adulthood, accounts for 80% of cases in adult female patients. Late-onset acne is defined as acne that begins after the age of 25 years.
- This problem in women can occur at any age and with varying degrees of severity. Women with signs of hyperandrogenism such as hirsutism or menstrual irregularities and those with true late-onset acne should be further evaluated for an underlying endocrine disorder such as PCOS.
- For most of those affected, the disorder is annoying and may be troublesome, but is not of enormous significance because it is limited in extent and only lasts a few months or at the most a year. For the unfortunate few, the condition is a disaster, as it is disfiguring, disabling and persistent, with wave after wave of new lesions.
- It improves in the summertime and sun exposure seems to improve the condition of many patients. However, the heat does not produce improvement and, indeed, can make it much worse
- Too much sebum in a follicle can cause a hardened plug to form, which can then lead to various forms of acne.
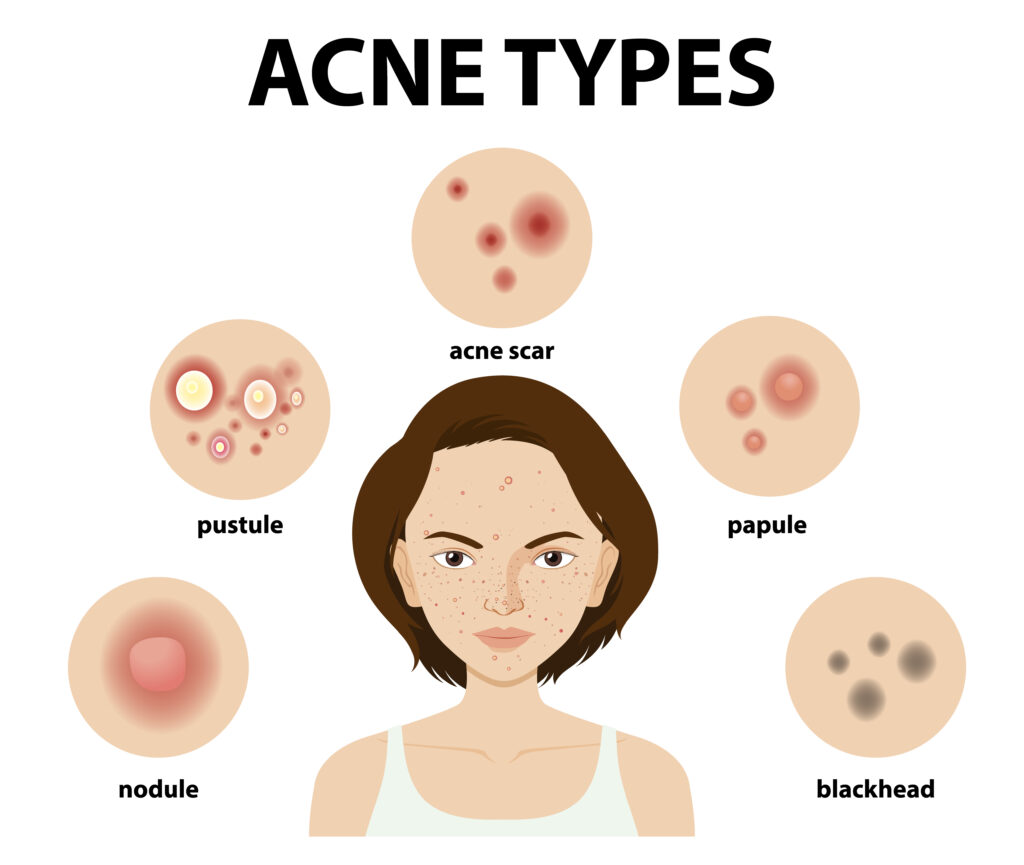
Different forms of acne include:
- Blackheads: Open pores on the skin filled with excess oil, dead skin, and hair. They get clogged by the dirt that causes them to appear as dark spots.
- Whiteheads: Bumps that remain closed by oil and dead skin.
- Papules: Small red or pink bumps initially that may become inflamed later.
- Pustules: Pimples filled with pus and can cause scarring if plucked or scratches. They look like whiteheads surrounded by red rings.
- Nodular: large and painful solid pimples that are deep in the skin.
- Cystic lesions: Pus-filled pimples that can cause scars.
Grading of acne based on the severity
- Grade 1 (mild): mostly whiteheads and blackheads, with a few papules and pustules.
- Grade 2 (moderate, or pustular acne): multiple papules and pustules, mostly on your face.
- Grade 3 (moderately severe, or nodulocystic acne): numerous papules and pustules, along with occasionally inflamed nodules. Your back and chest may also be affected.
- Grade 4 (severe nodulocystic acne): numerous large, painful, and inflamed pustules and nodules.
Differential Diagnosis
- Warts
- Acne Rosacea
- Seborrheic dermatitis
General Management
The best way to treat acne depends on how severe it is.
- Dietetic and social restrictions are typical, as is more frequent washing.
- Treatment may be aimed at:
- Reducing the bacterial population of the hair follicles to cut down the hydrolysis of lipids (antimicrobial agents). Encouraging the shedding of the follicular horny plugs to free the obstruction (comedolytic agents). reducing the rate of sebum production, either directly by acting on the sebaceous glands or indirectly by inhibiting the effects of androgens on the sebaceous glands (anti-androgens).
- Reducing the damaging effects of acne inflammation on the skin with anti-inflammatory agents.
- Patients with acne are often depressed and may need sympathetic counseling and support.
- There is no evidence that particular foodstuffs have any deleterious effect or that washing vigorously will help remove lesions. These and other myths should be dispelled and replaced with a straightforward explanation of the nature of the disorder, its natural history, and treatment.
Homeopathic Management

As Master Samuel Hahnemann said in his Organon of Medicine, 6th Edition, §173 “The only diseases that seem to have but few symptoms, and on that account to be less amenable to cure, are those which may be termed one-sided, because they display only one or two principal symptoms which obscure almost all the others. They belong chiefly to the class of chronic diseases”.
Acne, being an outward manifestation of internal malady has to be treated from its root cause, therefore it is necessary to administer proper similimum in order to achieve cure.
Based on individualization, there are various medicines in our materia medica that not only reduce the current symptoms of acne but also help in reducing the intensity and severity of acne lesions.
- Antim crudum.
- Hepar sulphuricum.
- Silicea.
- Kalium bromatum
- Kalium carbonicum
- Asteria rubens
- Calcarea silicatum
- Belladonna
- Sulphur
- Graphitis
- Dulcamara
- Pulsatilla
- Merc solubilis, etc


